Did you know that nearly 9% of the global population struggles with behaviors that go beyond just food? These mental health challenges are more complex than they appear, often rooted in a mix of genetic, psychological, and social factors.
Conditions like anorexia nervosa and binge eating are not just about food. They are serious health conditions that require attention and care. Early detection can make a significant difference, with recovery rates as high as 80% when treated promptly.
In this article, we’ll explore the signs, causes, and effective treatments for these challenges. You’ll learn about six primary types and three lesser-known variants. We’ll also dive into diagnostic criteria from the DSM-5-TR and treatment protocols from the Cleveland Clinic.
Key Takeaways
- Nearly 9% of the global population is affected by these behaviors.
- They involve genetic, psychological, and social factors.
- Early detection can lead to an 80% recovery rate.
- Six primary types and three lesser-known variants exist.
- Diagnostic criteria and treatment protocols are widely available.
Understanding Eating Disorders
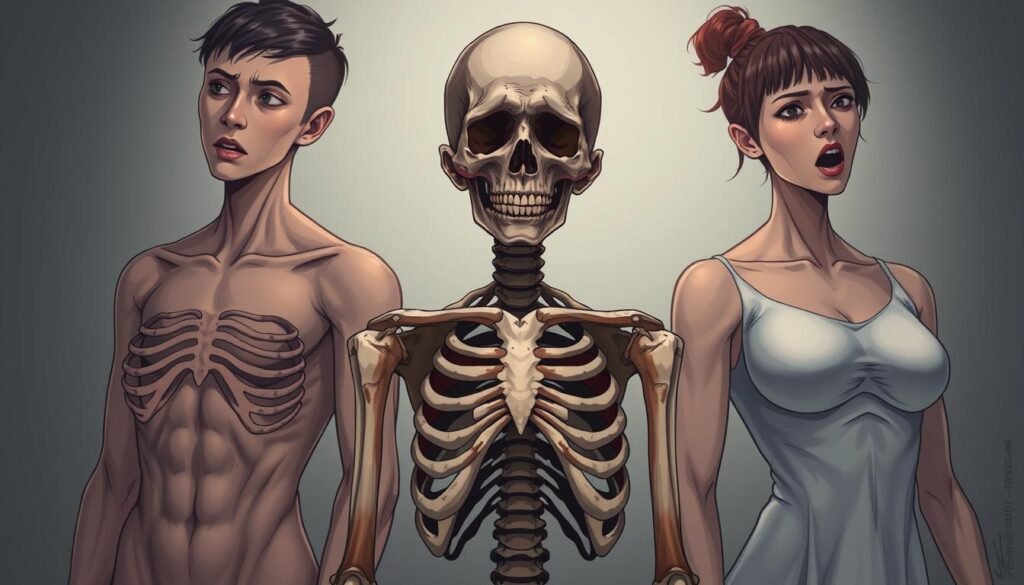
These conditions affect millions, blending biological, psychological, and social factors. They are not just about food but involve complex interactions that impact overall well-being. Recognizing the signs early can save lives and improve outcomes.
What Are Eating Disorders?
Eating disorders are bio-psycho-social conditions that require multidisciplinary care. They often stem from imbalances in neurotransmitters like serotonin and dopamine, which regulate mood and behavior. These imbalances can lead to severe disruptions in both mental health and physical well-being.
The Impact on Mental and Physical Health
The physical consequences are alarming. Conditions like anorexia can increase the risk of heart failure by 500%. Other effects include electrolyte imbalances, gastrointestinal damage, and osteoporosis. These health conditions can be life-threatening if left untreated.
Psychologically, these disorders often lead to social isolation, cognitive impairment, and even suicide risk. Nearly 50% of cases show comorbid depression or anxiety, making treatment more complex. In the U.S., these conditions contribute to over 10,200 annual deaths, highlighting their severity.
Addressing these challenges requires a holistic approach. Early intervention and comprehensive care can significantly improve outcomes. Understanding the full scope of these conditions is the first step toward effective treatment and recovery.
Types of Eating Disorders
Understanding the different forms of these conditions is crucial for effective care. Each type has unique characteristics and challenges. Recognizing them early can lead to better outcomes.
Anorexia Nervosa
Anorexia nervosa involves extreme food restriction and fear of weight gain. Some individuals maintain a normal weight, making it harder to detect. This condition can lead to severe health risks, including heart failure.
Bulimia Nervosa
Bulimia nervosa is marked by cycles of binge eating followed by purging. These episodes can occur up to 17 times weekly. Vomiting and laxative use are common methods of purging.
Binge Eating Disorder (BED)
Binge eating disorder affects 2.8% of U.S. adults. It involves consuming large amounts of food without purging. This behavior increases the risk of metabolic syndrome and diabetes.
Pica
Pica involves consuming non-food items like laundry detergent. It affects 10-32% of children with developmental disabilities. This condition can lead to serious health complications.
Rumination Disorder
This condition involves repeatedly regurgitating food. It can lead to malnutrition and weight loss. Early intervention is key to managing symptoms.
Avoidant/Restrictive Food Intake Disorder (ARFID)
Avoidant restrictive food intake disorder is linked to sensory-based food avoidance. Its prevalence has increased by 300% in pediatric populations since 2010. This condition can lead to nutritional deficiencies.
Signs and Symptoms of Eating Disorders
Identifying the symptoms of these health challenges is the first step toward recovery. These conditions often manifest in physical, behavioral, and emotional ways. Recognizing these signs early can lead to timely intervention and better outcomes.
Physical Symptoms
Physical markers can vary widely. For example, 73% of cases show lanugo hair growth, a fine hair that develops due to malnutrition. Another common sign is Russell’s Sign, seen in 68% of cases, which involves calluses on the hands from repeated vomiting.
Other physical symptoms include amenorrhea (loss of menstrual periods), dental erosion, and esophageal tears. These issues highlight the severe impact on overall health.
Behavioral and Emotional Symptoms
Behavioral red flags often include food rituals, excessive exercise, and laxative abuse. These actions can indicate a deeper struggle with body image and control.
Emotionally, people may engage in body checking, social withdrawal, or meal avoidance. These behaviors can lead to isolation and worsen the condition.
Diagnostic timelines show that symptoms typically emerge over 6-24 months. Gender-specific presentations, like muscle dysmorphia in males, further complicate detection.
Causes of Eating Disorders
The roots of these health challenges are deeply intertwined with genetics, psychology, and societal pressures. Understanding these causes can help in prevention and treatment.
Genetic Factors
Research shows that genetic factors play a significant role. First-degree relatives have a 12x higher risk of developing similar conditions. The heritability rate for anorexia is around 40%, indicating a strong genetic link.
Specific gene variants, like COMT, affect dopamine processing. This can influence mood and behavior, increasing the likelihood of these health challenges.
Psychological Factors
Psychological factors are equally important. Trauma, such as childhood abuse, is reported in 45% of cases. These experiences can lead to coping mechanisms that manifest as harmful behaviors.
Additionally, conditions like depression and anxiety often coexist, complicating the diagnosis and treatment process.
Social and Environmental Influences
Social environmental influences also contribute significantly. Social media use for more than 3 hours daily increases the risk by 60%. The $72 billion weight loss industry promotes unrealistic body standards, adding to the pressure.
In sports, 25% of gymnasts develop these conditions due to the intense focus on weight and performance. These external factors highlight the need for awareness and intervention.
Diagnosing Eating Disorders
Accurate diagnosis is the cornerstone of effective treatment for these health challenges. A thorough evaluation involves both medical evaluations and psychological assessments. This dual approach ensures a comprehensive understanding of the condition and its underlying causes.
Medical Evaluations
Medical evaluations are essential to identify physical symptoms and complications. Common lab tests include CBC, BMP, TSH, and ECG. These tests help detect imbalances in albumin, prealbumin, and phosphorus levels, which are critical biomarkers.
Imaging studies, such as MRI, can reveal structural changes like grey matter loss in individuals with anorexia. These findings provide valuable insights into the condition’s impact on the brain and overall health.
Psychological Assessments
Psychological assessments play a vital role in understanding behavioral and emotional patterns. Tools like the EDE-Q questionnaire show 92% diagnostic accuracy. The SCOFF questionnaire and CEDS-R are also widely used for screening and evaluation.
Comorbidity challenges, such as distinguishing these conditions from OCD or depression, require careful analysis. Early and precise identification can significantly improve recovery outcomes for people affected by these health challenges.
Effective Treatments for Eating Disorders
Effective approaches to managing these health challenges focus on tailored interventions and comprehensive care. A combination of therapies, medical support, and lifestyle changes can significantly improve outcomes. Let’s explore the most effective treatments available today.
Psychotherapy
Psychotherapy is a cornerstone of treatment, with Family-Based Therapy (FBT) showing a 75% success rate in adolescents. Cognitive Behavioral Therapy (CBT-E) and Dialectical Behavior Therapy (DBT) are also highly effective. These therapies address underlying psychological factors and promote healthier behaviors.
Medical and Nutritional Support
Medical and nutritional support is crucial for restoring physical health. Refeeding protocols often start at 1200kcal, with careful monitoring of phosphorus levels. This approach helps prevent complications like refeeding syndrome, ensuring a safer recovery process.
Medication
Medications like SSRIs are commonly used for bulimia, while Vyvanse is effective for binge eating. Olanzapine has been shown to reduce anorexia relapse by 40%. These medications work alongside therapy to address both physical and psychological symptoms.
Hospitalization and Residential Treatment
In severe cases, hospitalization or residential treatment may be necessary. Criteria include being below 75% of ideal body weight or having a QTc interval over 470ms. Tube feeding may be required in critical situations to stabilize the patient’s health.
Each treatment plan is tailored to the individual’s needs, ensuring the best possible path to recovery. Early intervention and a multidisciplinary approach are key to long-term success.
Recovery and Management
Recovery from these health challenges is a journey that requires patience, support, and a well-structured plan. Studies show that 50% of people achieve full recovery within 10 years, highlighting the importance of consistent effort and care. A combination of professional guidance, personal commitment, and a strong support system can make a significant difference.
Building a Support System
A strong support system is crucial for successful recovery. Family, friends, and healthcare professionals play a vital role in providing encouragement and accountability. Family-Based Therapy (FBT) has shown a 75% success rate in adolescents, emphasizing the importance of involving loved ones in the process.
Developing Healthy Eating Habits
Meal support can reduce relapse rates by 35%, making it a key component of recovery. Creating structured meal plans and using tools like smartphone apps (e.g., Recovery Record or Rise Up) can help establish healthy eating habits. These apps offer tracking features and reminders to support daily progress.
Long-Term Management Strategies
For long-term management, it’s essential to set realistic goals and milestones. A 5-year recovery roadmap can help track progress and celebrate achievements. Harm reduction strategies are also important for chronic cases, focusing on minimizing risks while promoting overall well-being.
Workplace and school accommodations, such as flexible schedules or meal breaks, can further support recovery. These adjustments ensure that individuals have the resources they need to thrive in their daily lives.
Preventing Eating Disorders
Preventing these health challenges starts with awareness and proactive measures. By addressing risk factors early and promoting healthy behaviors, we can reduce the likelihood of these conditions developing. Schools, communities, and families all play a vital role in fostering environments that support mental and physical well-being.
Early Intervention
Early intervention is key to reducing the onset of these conditions. School-based programs have been shown to decrease the likelihood by 29%, according to the NIMH. These programs focus on educating students about healthy habits and providing resources for those at risk.
Media literacy is another powerful tool, cutting risk factors by 40%. Teaching individuals to critically analyze media messages helps them resist unrealistic body standards and societal pressures.
Promoting Positive Body Image
Encouraging a positive body image is essential for prevention. The HAES® (Health At Every Size) approach has shown promising outcomes by focusing on self-acceptance and holistic health rather than weight. Social media detox protocols can also help individuals break free from harmful comparisons and foster self-esteem.
Educational Programs
Educational programs are a cornerstone of prevention efforts. NEDA’s 7-step framework provides a comprehensive guide for schools and communities to implement effective strategies. These steps include promoting healthy eating, addressing bullying, and fostering open conversations about mental health.
The anti-diet movement has also gained traction, challenging harmful diet culture and encouraging intuitive eating. Corporate responsibility guidelines for fashion and beauty industries further support these efforts by promoting diverse and realistic body representations.
Living with an Eating Disorder
Living with these challenges requires resilience and a proactive approach to managing daily life. Many individuals find that with the right strategies and support, they can navigate their journey toward recovery effectively. This section explores practical ways to cope, build a supportive network, and handle everyday obstacles.
Coping Mechanisms
Developing effective coping mechanisms is essential for managing stress and triggers. Exposure therapy, for example, has been shown to reduce meal anxiety by 60%. Techniques like mindfulness, journaling, and structured meal planning can also provide stability and reduce the risk of relapse.
Finding Community Support
Building a strong community support system can significantly improve quality of life. Studies show that 82% of individuals report better outcomes when they connect with peers who understand their struggles. Online forums, support groups, and therapy sessions can offer valuable encouragement and accountability.
Navigating Daily Challenges
Everyday situations, like dining out or traveling, can be daunting. A restaurant survival guide with meal planning templates can help reduce anxiety. Workplace accommodations, such as flexible schedules, and travel strategies, like packing safe snacks, ensure that recovery remains a priority in all settings.
Understanding ADA protections and seeking workplace accommodation letters can also provide legal support. For chronic sufferers, harm reduction strategies focus on minimizing risks while promoting overall well-being. These practical steps empower individuals to face daily challenges with confidence.
Conclusion
Recovery is not just possible—it’s achievable with the right support and resources. Studies show that 90% of individuals see significant improvement with early intervention and proper treatment. If you or someone you know is struggling, reaching out for help is the first step toward healing.
For immediate assistance, contact the NEDA Helpline at 800-931-2237 or text “HELP” to the Crisis Text Line. These resources provide confidential support and guidance. Taking action early can make a life-changing difference.
Here are five steps to consider if you suspect a loved one is affected: 1) Educate yourself about the condition, 2) Approach them with compassion, 3) Encourage professional evaluation, 4) Offer consistent support, and 5) Connect them with specialized care. Small steps can lead to big changes.
Success stories highlight the power of perseverance. Ten-year follow-up data reveals that many individuals achieve full recovery, reclaiming their health and happiness. Every journey is unique, but hope is a constant.
Remember, recovery is a process, not a destination. With the right tools and support, a brighter future is within reach.
FAQ
What are the most common types of eating disorders?
The most common types include anorexia nervosa, bulimia nervosa, binge eating disorder (BED), pica, rumination disorder, and avoidant/restrictive food intake disorder (ARFID). Each has unique characteristics and behaviors.
What are the physical symptoms of an eating disorder?
Physical symptoms may include extreme weight loss, fatigue, dizziness, irregular heartbeats, and digestive issues. Severe cases can lead to organ damage or life-threatening conditions.
What causes eating disorders?
Causes are complex and often involve a combination of genetic, psychological, and social factors. Trauma, societal pressures, and family history can also play significant roles.
How are eating disorders diagnosed?
Diagnosis typically involves medical evaluations, psychological assessments, and discussions about eating habits, body image, and emotional well-being with a healthcare professional.
What treatments are available for eating disorders?
Effective treatments include psychotherapy, medical and nutritional support, medication, and in severe cases, hospitalization or residential treatment programs tailored to individual needs.
Can eating disorders be prevented?
Early intervention, promoting positive body image, and educational programs can help reduce the risk. Encouraging healthy relationships with food and self-esteem is also crucial.
How can someone support a loved one with an eating disorder?
Offer empathy, avoid judgment, and encourage professional help. Building a strong support system and educating yourself about the condition can make a significant difference.
What are the long-term management strategies for recovery?
Long-term strategies include ongoing therapy, developing healthy eating habits, staying connected with support groups, and addressing underlying emotional or psychological challenges.
Are there medications that help with eating disorders?
Certain medications, such as antidepressants or anti-anxiety drugs, may be prescribed to manage symptoms, especially when combined with therapy and nutritional support.
What is the role of psychotherapy in treating eating disorders?
Psychotherapy, such as cognitive-behavioral therapy (CBT), helps individuals address unhealthy thought patterns, behaviors, and emotions related to food, body image, and self-worth.